1.7 Pre-Birth Procedures and Guidance
This procedure was updated on 23/06/22 and is currently uptodate.
Contents
- Principles of the Pre Birth Procedure(Jump to)
- Guidance for all Agencies(Jump to)
- Continuum of Need Incorporating Threshold Guidance(Jump to)
- Early Screening for vulnerabilities(Jump to)
- Information Sharing and Consent(Jump to)
- Fraser Guidelines(Jump to)
- Responding to Concealed or Denied Pregnancy(Jump to)
- Referral where vulnerability is indicated(Jump to)
- Early Help assessment and support(Jump to)
- Risk of significant harm(Jump to)
- Post Birth Planning(Jump to)
- Related Policies, Procedures and Guidance(Jump to)
- Useful References(Jump to)
- Appendix(Jump to)
Principles of the Pre Birth Procedure
| 1.7.1 | Principles of the Pre Birth Procedure This Pre Birth Procedure has been developed and designed by a multi-agency group, established under the Buckinghamshire Safeguarding Children Partnership (BSCP) in order to develop a consistent Pre Birth Assessment Pathway which identifies vulnerability early and provides a clear route into appropriate support services. The group have taken into account findings from local Learning Lessons and Serious Case Reviews as well as local and national research into good practice. The key principles of the Buckinghamshire Safeguarding Children Partnership (BSCP) Pre Birth Assessment Procedure are:
All staff to be aware that if at any point there is disagreement about the correct level of intervention reference should be made to the BSCB Escalation, Challenge and Conflict Resolution procedure. |
Guidance for all Agencies
Think Pregnancy - Think Midwifery | |
| 1.7.2 | All women who suspect that they may be pregnant should be advised to book in with Midwifery at the earliest opportunity. This is usually between 8-10 weeks of pregnancy if the pregnancy has been notified to the Midwife. The booking appointment should be no later than the end of week 12. Other professionals must not assume that a family is known to Midwifery Services. If any agency becomes aware that a woman is pregnant then contact needs to be made with Midwifery for booking in at the earliest opportunity. Evidence indicates that women who have additional vulnerability are less likely to access antenatal care or stay in regular contact with maternity services. Where vulnerability has been identified, providing antenatal services in a more flexible way may encourage women to attend more regularly and therefore receive appropriate care and referrals. For further information please see Pregnancy and Complex Social Factors, NICE guidelines CG110, (2010) (Revised 2018) If there are immediate concerns about an unborn child or an adult with care and support needs, existing safeguarding procedures need to be followed alongside encouragement to access maternity services. |
Continuum of Need Incorporating Threshold Guidance
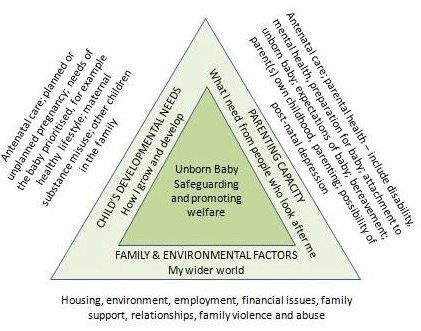
| 1.7.3 | The Continuum of Need document replaces the BSCP Threshold Guidance as of March 2021 and is to be used as the Partnership tool in assessing need. The Pre Birth Pathway follows the Continuum of Need document 2021 and describes 4 types of response to meeting the needs of children and families. As needs are identified and assessed during pregnancy, there should be consideration of a ‘step up or step down’ approach to safeguard the unborn baby and the parent/parents so are supported by the most appropriate services. |
Universal Services - Continuum of Need Incorporating Threshold Guidance | |
| 1.7.4 | No additional needs identified or limited intervention to avoid needs arising. Children and young people whose needs are met by on-going services such as schools, GP’s, Health visitors and Dentist alongside the love, care and protection of parents and carers. Children and young people in this category are making good overall progress in all areas of their development. Some limited intervention from a universal service may be needed to avoid needs arising or to meet a single identified need. The majority of children living in each local authority area will fall into this category. |
| 1.7.5 | Think Pregnancy – Think Midwifery - All women who suspect that they may be pregnant should be advised to book in with Midwifery at the earliest opportunity. This is usually between 8-10 weeks of pregnancy if the pregnancy has been notified to the Midwife. The booking appointment should be no later than the end of week 12. Other professionals must not assume that a family is known to Midwifery Services. If any agency becomes aware that a woman is pregnant then contact needs to be made with Midwifery for booking in at the earliest opportunity. Evidence indicates that women who have additional vulnerability are less likely to access antenatal care or stay in regular contact with maternity services. Where vulnerability has been identified, providing antenatal services in a more flexible way may encourage women to attend more regularly and therefore receive appropriate care and referrals. For further information please see Pregnancy and Complex Social Factors, NICE guidelines CG110, (2010) (Revised 2018) If there are immediate concerns about an unborn child or an adult with care and support needs, existing safeguarding procedures need to be followed alongside encouragement to access maternity services. |
The Continuum of Need document replaces the BSCP Threshold Guidance as of March 2021 and is to be used as the Partnership tool in assessing need. The Pre Birth Pathway follows the Continuum of Need document 2021 and describes 4 types of response to meeting the needs of children and families. As needs are identified and assessed during pregnancy, there should be consideration of a ‘step up or step down’ approach to safeguard the unborn baby and the parent/parents so are supported by the most appropriate services. | |
| 1.7.6 | Universal Services (Level 1) No additional needs identified or limited intervention to avoid needs arising. Children and young people whose needs are met by on-going services such as schools, GP’s, Health visitors and Dentist alongside the love, care and protection of parents and carers. Children and young people in this category are making good overall progress in all areas of their development. Some limited intervention from a universal service may be needed to avoid needs arising or to meet a single identified need. The majority of children living in each local authority area will fall into this category. Additional Services (Level 2)Additional Need - Children and young people with additional needs (not just SEN), that can be met through a single agency response or agencies working together to provide a coordinated partnership response. The support required may be only short term, but if ignored these issues could lead to escalation. Comprehensive Support (Level 3) Children and young people who have multiple and complex needs requiring a multi-agency Early Help response with a lead professional. Level 3 also includes the threshold for a Child in Need. Although a Child in Need requires a statutory response from Children’s Social Care, a statutory intervention is not necessarily required. For this reason, the threshold for a Child in Need falls in level 3, but where a statutory intervention is required from Children’s Social Care this would fall into level 4. It should be noted that at this level Early Help involvement is still an option. Children and young people in this category have increasing levels of un-met needs that are more significant and complex. The range, depth or significance of the problems faced by children at level 3 may begin to prevent them from achieving or maintaining a reasonable standard of health or development if they don’t receive appropriate services. They are likely to require targeted and/or longer-term intervention from specialist services Statutory Specialist Support (Level 4) Children and young people with a high level of unmet or complex needs or children who are in need of protection. Children and young people in this category are identified as having suffered or likely to be suffering significant harm or significant impairment to their health or development. Harm is defined under 4 possible categories: physical abuse, emotional abuse, sexual abuse and neglect. These children require intensive support under Section 47 of the Children Act 1989 (Child Protection Plan). Sometimes ‘Significant Harm’ will be a single, traumatic event, but more often it is an accumulation of significant events, both acute and longstanding over time, such as in situations of neglect. |
Early Screening for vulnerabilities
| 1.7.7 | Ante Natal care for uncomplicated pregnancies (NICE CG62 2008) (updated 2019) outlines routine maternity care for healthy pregnant women. Pregnant women with complex social factors may have additional needs. The Pregnancy and Complex social factors (NICE CG110) (updated 2010) contain a number of recommendations on standards of care for all pregnant women with complex needs. These guidelines set out what healthcare professionals, and antenatal services, can do to address the needs and improve pregnancy outcomes in this group of women. Midwives are well placed to gather important information about expectant mothers and their circumstances, early in the pregnancy. A booking interview is carried out at around 8-10 weeks of pregnancy either in the woman’s home or at a location of her choice (for example the GP surgery, maternity unit or local Children’s Centre). During the booking interview, the lead midwife responsible for the patient’s care collects information to build into a full medical and social history. This data helps the midwife to assist the woman in making informed choices about the care she receives and to offer advice on the suitability of her choices. The midwife will discuss with the woman the pattern of care which is most suited to her needs and will work with her to develop a safe plan of care based on her preferences. A holistic approach, taking into account the woman’s social history is provided. Gathering this information assists with identifying mothers for whom there are complex social factors that may impact on her and her partner’s parenting capacity. This information will be incorporated into a pre-birth assessment where appropriate. Midwifery services will share information with the Health Visitor/Family Nurse during the pregnancy. Within Buckinghamshire, the Health Visitor/Family Nurse will complete an antenatal visit for all mothers between 28 and 32 weeks. It is important that the named Health Visitor/Family Nurse is part of the pre-birth assessment. Midwives may identify that a mother has, or may have been, subjected to female genital mutilation (FGM). FGM can lead to birth complications such as prolonged labour, recourse to caesarean section, postpartum haemorrhage and tearing. If FGM is identified, professionals must follow the procedures as set out in the guidelines developed by their agencies and BSCP’s Female Genital Mutilation (FGM) – Guidance Buckinghamshire Healthcare NHS Trust Midwives meet regularly with Health Visitors/Family Nurses and GP’s to share information to ensure that mothers are accessing appropriate care. They will escalate any concerns to safeguarding leads within their own agencies, and to the relevant social worker. Bucks CCG has commissioned and developed a universal, NICE (CG 192) compliant pathway for perinatal mental health :- https://www.oxfordhealth.nhs.uk/buckinghamshire-perinatal-mental-health-service/ https://www.oxfordhealth.nhs.uk/service_description/adult-community-mental-health-teams/ GPs, Midwives and Health Visitors/Family Nurses are uniquely placed to screen for risk factors during the perinatal period. Prompt identification, assessment and treatment with referral to the most appropriate services will reduce the impact of the disorders on the mother, her child and family. The Buckinghamshire multi-agency perinatal mental health network comprises partners from general practice, commissioning, Midwifery, Health Visiting, CAMHS, ReConnect (parent-infant service which works with parents and children with disorganised attachment issues), Healthy Minds (Psychological Services) and Adult Mental Health. Its aim is to deliver accessible universal services to support women and families across the county when there are perinatal mental health concerns. Parents with learning disabilities or difficulties Parents may sometimes require extra help to manage caring for a young child – ‘a learning disability affects the way a person understands information and how they communicate. This means they can have difficulty understanding new or complex information, learning new skills and coping independently. Around 1.5 million people in the UK have a learning disability.’(https://www.nhs.uk/conditions/learning-disabilities/ ). The UK legislative framework dictates that parents with learning difficulties have a right to have children and to be supported in bringing them up. However, it is recognised that such parents will face a particular set of problems and challenges, including accessing antenatal care, understanding information about their pregnancy and birth choices or medical information about their baby. Parents may also be anxious about asking for or accepting professional help as they may believe that this will result in their child being removed from their care. Malouf et al (2016) concluded: ‘Mothers who will be subject to a social care assessment of their parenting skills need clear information about the process, their choices and the level of skill they must demonstrate, as well as access to sufficient antenatal and postnatal support…’ If the parents of the unborn child are already accessing support via adult services the lead worker must be involved in any pre-birth assessment. If adult services are not involved this should be explored with the parents and, with consent, a referral could be made for additional support. Parents with significant physical health problems or disabilities It may be difficult for them to care for a young child - there are around 1.7 million disabled parents in the UK, mostly with physical and sensory impairments. A report on a UK study on physically disabled parents' experiences of maternity services reveals that physically disabled people embarking on parenthood face a number of challenges in getting appropriate information and support, including negative attitudes from some health professionals, a lack of knowledge and information available for parents and professionals, as well as poor communication between disabled parents and professionals. Parents who are Looked After or Care Leavers Some of the key risk factors associated with teenage pregnancy are particularly apposite for young people who are looked after or care leavers. Pregnant teenagers who are looked after/care leavers will often need significant support and guidance to enable them to make informed choices about their future and should be put in contact with relevant health professionals at the earliest opportunity (including specialist teenage pregnancy services where these are available and appropriate). For young people who are looked after by the local authority, the Social Worker will have primary responsibility for ensuring access to services and the coordination and updating of the Care Plan in relation to either or both young parents. All pregnant children in care will be known to the children’s looked after specialist nurses and they should be included in the holistic early help / assessment process. In addition all children in care or care leavers up to age 20 at conception will be offered the Family Nurse Partnership programme as per the notification pathway Asylum seekers and families where English is not a first language Migrants, refugees and asylum seeking women who have recently arrived into the UK bring a range of complexities for services to address. The key issues include poor overall health status, language difficulties as many do not speak English, underlying and possible unrecognised medical conditions and HIV/AIDS and TB It is always important that the use of Interpreters should always be adhered to as per organisation policy and guidance. Please see link for Language interpretation: migrant health guidance. https://www.gov.uk/guidance/language-interpretation-migrant-health-guide It is important that there is awareness on statistics and that there is a five-fold difference in maternal mortality rates amongst women from Black ethnic backgrounds and an almost two-fold difference amongst women from Asian Ethnic backgrounds compared to white women (Knight et al, 2018). There are also significant adverse pregnancy outcomes for babies. Families who are homeless Women who are pregnant and homeless are a concerning group of women who are at significant risk of adverse foetal and maternal outcomes. Women often become homeless due to family breakdown, debt, poor mental health and substance misuse problems, domestic abuse and often through no fault of their own which adds considerably to their vulnerability and those of the unborn infant. It becomes crucial that very robust collaborative working is needed by all who provide social and healthcare services to homeless pregnant women, to improve the health outcomes for these women and babies. Working with Fathers It is important that all agencies involved in pre and post birth assessment and support, fully consider the significant role of fathers and wider family members in the care of the baby even if the parents are not living together and where possible involve them in the assessment. This should include the father's attitude towards the pregnancy, the mother and new born child and his thoughts, feelings and expectations about becoming a parent. Information should also be gathered about fathers and partners who are not the biological father at the earliest opportunity to ensure any risk factors can be identified. Failure to establish Information regarding the father may mean that practitioners are not able to accurately assess what mothers and other family members might be saying about the father's role, the contribution which they may make to the care of the baby and support of the mother, or the risks which they might present to them. Background Police and other checks should be made at an early stage on relevant cases to ascertain any potential risk factors. Involving fathers in a positive way is important in ensuring a comprehensive assessment can be carried out and any possible risks fully considered. Pregnancy and coronavirus (Relevant for 2020-2021) There's no evidence that pregnant women are more likely to get seriously ill from coronavirus. Pregnant women have been included in the list of people at moderate risk (clinically vulnerable) as a precaution. This is because pregnant women can sometimes be more at risk from viruses like flu. It’s not clear if this happens with coronavirus. But because it's a new virus, it's safer to include pregnant women in the moderate-risk group. There’s no evidence coronavirus causes miscarriage or affects how a baby develops in pregnancy. (https://www.nhs.uk/conditions/coronavirus-covid-19/people-at-higher-risk/pregnancy-and-coronavirus/ ) Adverse Childhood Experiences Adverse Childhood Experiences (ACEs) is the term used to describe traumatic experiences before age 18 that can lead to negative, lifelong emotional and physical outcomes. When the stress of these adverse experiences is so severe or prolonged that a child is unable to process it, what should be a normal survival response becomes “toxic stress”. This type of stress alters the functioning of the brain and has a long-lasting and injurious impact on the developing mind, which we call “trauma”. This trauma affects the way those suffering it think and act throughout their lives. Understanding such mental and emotional trauma is key to understanding the behaviour of millions of people. The term ACEs derives from a study carried out in the 1990s in California. The 10 ACEs they measured were to do with Abuse, Neglect and household dysfunction including divorce, domestic abuse, parent in prison, mental illness and substance misuse. This list is not exhaustive and there are other types of adverse childhood experiences not included in the list of 10 ACEs above, including community and environmental ACEs such as racism, bullying and community violence. Parental behaviours which may pose a risk to a child Domestic abuse: is a complex global public health problem as well as a violation against human rights. WHO’s (World Health Organisation) definition where it is defined as physical, sexual or psychological, or emotional violence, or threats of physical or sexual violence that are inflicted on a pregnant woman by a family member, i.e. an intimate male partner, marital/cohabiting partner, parents, siblings, or a person very well known to the family, or a significant other, (i.e. former partner) when such violence often takes place in the home. Pregnancy can be both a trigger and risk factor for domestic abuse with domestic abuse starting or intensifying in pregnancy. Between 4% and 9% of women are abused during pregnancy and/or after the birth (Taft 2002). Domestic abuse is associated with an increased risk of miscarriage, still birth and premature birth (NHS 2018). It is can also be linked to mental health concerns and substance usage (DH, 2010). Domestic abuse also directly affects the unborn baby: by 18 weeks gestation the unborn baby can hear and by 24-26 weeks gestation the unborn will be startled by very loud noises outside the womb which can cause a stress response in the baby. If a pregnant woman is stressed or scared over a significant period of time, which often occurs where there is domestic abuse, increased levels of the stress hormone, cortisol, will be shared with the unborn baby. Cortisol affects the brain development of the unborn baby and has been associated with mental health concerns later in life as well as affecting the growth of the unborn baby. The effects on babies/children of exposure to family violence are similar to those for children who have been abused. Substance misuse by mothers/parents does not on its own automatically indicate that children are at risk of abuse or neglect. However, where substance misuse is causing physical, psychological, social, interpersonal, financial and or legal problems, the implications for children and families must be thoroughly assessed. Drug and alcohol misuse during pregnancy, dependent on frequency and severity, can adversely impact the developing foetus, particularly during the first twelve weeks of gestation. Risks include increased risk of miscarriage, likelihood of premature delivery, reduced birthweight and head circumference, and an increased risk of Sudden unexpected death in infancy. The infant exposed to drug or alcohol use during pregnancy may also experience additional long-term cognitive and development problems. Parental mental illness During pregnancy and in the year after birth, women can be affected by a range of mental health problems, including anxiety, depression and postnatal psychotic disorders. These are collectively called perinatal mental illnesses. Perinatal mental Illnesses are the most common complication of childbearing affecting approximately 10-15% of women and as such represents a considerable public health problem affecting women and their families (Warner et al., 1996) and between a quarter and half of fathers with a partner with a perinatal mental illness are depressed themselves (J Goodman 2004). The number of men who become depressed in the first year after becoming a dad is double that of the general population. First time dads are particularly vulnerable. One in ten dads-to-be will also become depressed during their partner’s pregnancy. https://www.nct.org.uk/life-parent/emotions/postnatal-depression-dads-10-things-you-should-know Some women are at an increased risk of experiencing mental illness in the perinatal period, particularly those who have had a previous history of mental illness. A small group of women are known to be at significant risk of developing severe perinatal mental illness. Women who have experienced postpartum psychosis, severe depression in the past or have a diagnosis of Bi-polar disorder have around a 50% chance of becoming unwell in the perinatal period (Oates, M, 2001; Jones, 2019). Most families where there is perinatal mental illness manage very well and are able to give their children safe and loving care. However, without the right support, perinatal mental illness can have an adverse effect on the baby’s brain development and long-term outcomes for the child (Centre on the Developing Child at Harvard University 2009). Interactions with caregivers are the most important element of a baby’s early experience and help build secure and stable attachments. The nature of this early attachment sets the template for future relationships and can predict a number of physical, social, emotional and cognitive outcomes (Cuthbert et al 2011). In more serious cases, parental mental illness increases the risk that a baby could be abused or neglected. Babies are particularly at risk if:
Much of the negative impact that parental perinatal mental health could have on the family and baby’s lives can be prevented. The quality of parent’s interactions with babies and the development of secure and stable attachment relationships can be improved through effective interventions (Hogg 2013). Maternal ambivalence affects some women. Almond (2011) defines maternal ambivalence. as that mixture of loving and hating feelings that all mothers experience towards their children, and the anxiety, shame and guilt that the negative feelings engender in them. A triennial analysis of serious case reviews (DfE, May 2016) recognised that maternal ambivalence towards her child (both during and after pregnancy) was highlighted in many reviews as a potential indicator of a child’s vulnerability. This could present as an unwanted pregnancy, or ambivalent feelings about being pregnant; and result in late antenatal booking, or non-engagement with antenatal services. Later presentations included an apparent lack of joy or warmth in relation to their baby. Whilst such cases are rare, other presentations including delayed antenatal booking or uncertainty about keeping the pregnancy are far more common. The report concluded that such presentations offer professionals (particularly in primary care and maternity services) opportunities to explore parental concerns and feelings towards the pregnancy and the unborn infant. A parent who presents as ambivalent about their pregnancy, or who does not seem to be engaging with parenthood provides an opportunity to explore with that parent, their feelings towards the child and any risks that this might pose (DfE2016). Parents with Autism Guidance from the National Autistic Society recommends the following in terms of interacting with autistic individuals: https://www.birthbabyparent.com/autisticandpregnantresources The below are also provided for guidance:- Surrogacy - government guidance in respect of surrogacy (2018) advises: Altruistic surrogacy is an established and legal way of creating a family in the UK. Surrogacy agreements are not legally enforceable and the IPs (intended parents) need to apply for a parental order after their child is born in order to become the legal parents of the child. The legal framework allows for a surrogate to receive reasonable pregnancy-related expenses from IPs, as assessed by the family court. Surrogacy through commercial means, however, is illegal in the UK (Surrogacy Arrangements Act 1985) and therefore it is an offence for an individual or agency to act on a profit-making basis to organise or facilitate surrogacy for another person. Any persons or organisations that organise or facilitate surrogacy must do so on a non-commercial basis.’ When any professional is made aware of a pregnancy as a result of a surrogacy arrangement they should seek advice from their Designated Officer for Safeguarding Children or the Designated/Named Doctor or Nurse with responsibility for safeguarding children, to enable them to make the necessary enquiries to satisfy themselves of the legitimacy of the arrangement. If professionals, following such consultation, are satisfied that the relevant Code of Practice (HFEA, 2017) has been followed, the local authority need not be informed unless there are other concerns being expressed that might indicate that the child may be at risk. Where the circumstances of the conception and subsequent arrangements for the baby are not clear the parents should be informed of the need for a referral to Children’s Social Care to allow for further enquiries to be made. |
Information Sharing and Consent
| 1.7.8 | Careful consideration must be paid to issues of consent and information sharing throughout any involvement with families. Parents should be informed as soon as possible of the concerns and the need for a referral to Early Help or Children’s Services, except on the rare occasions where doing so may increase the risk to the unborn baby and/or mother or jeopardise evidential information. Information sharing is vital to safeguarding and promoting the welfare of children and young people. A key factor identified in many serious case reviews (SCRs) has been a failure by practitioners to record information, to share it, to understand its significance and then take appropriate action. (DfE 2015). The DfE’s Information Sharing (Advice for Practitioners providing safeguarding services to Children, Young People, parents and carers) provides guidance on sharing information and includes the ‘Seven golden rules to sharing information. Professionals should also refer to the BSCP Information Sharing Code of Practice Other points to consider:
Seeking information/advice and timely sharing of information between agencies is vital to ensure the best use of the available professional expertise to facilitate decision making in the context of effective multi-agency working. It is each practitioner’s responsibility to familiarise themselves with internal mechanisms of reporting, sharing information and escalation of concerns. |
Fraser Guidelines
| 1.7.9 | When trying to decide whether a child / young person is mature enough to make decisions, people often talk about whether a child meets the Fraser Guidelines. The Fraser guidelines help to balance children’s rights and wishes with the responsibility to keep children safe from harm. The Fraser guidelines refer to a legal case which looked specifically at whether doctors should be able to give contraceptive advice or treatment to under 16 year olds without parental consent. However since then, they have been more widely used to help assess whether a child / young person has the maturity to make their own decisions and to understand the implications of those decisions (NSPCC, 2016).
|
Responding to Concealed or Denied Pregnancy
| 1.7.10 | The concealment and denial of pregnancy will present a significant challenge to professionals in safeguarding the welfare and wellbeing of the foetus (unborn child) and the mother. Concealment and denial limit the scope of professional help, better outcomes can be achieved by co-ordinating an effective inter-agency approach. This approach begins when a concealment or denial of pregnancy is suspected or in some cases when the fact of the pregnancy (or birth) has been established. This will also apply to future pregnancies where it is known or suspected that a previous pregnancy was concealed. A concealed pregnancy is when a woman knows she is pregnant but does not tell any health professional; or when she tells another professional but conceals the fact that she is not accessing antenatal care; or when a pregnant woman tells another person or persons and they conceal the fact from all health agencies. A denied pregnancy is when a woman is unaware of or unable to accept the existence of her pregnancy. Physical changes to the body may not be present or misconstrued; they may be intellectually aware of the pregnancy but continue to think, feel and behave as though they were not pregnant. In some cases a woman may be in denial of her pregnancy because of mental illness, substance misuse or as a result of a history of loss of a child or children (Spinelli, 2005). A pregnancy will not be considered to be concealed or denied for the purpose of these procedures and guidance until it is confirmed to be at least 24 weeks; this is the point of viability. However by the very nature of concealment or denial it is not possible for anyone suspecting a woman of concealing or denying a pregnancy to be certain of the stage the pregnancy is at. Where there is a strong suspicion there is a concealed or denied pregnancy, then it is necessary to share this irrespective of whether consent to disclose can be obtained or has been given. In these circumstances the welfare of the unborn child will override the mother’s right to confidentiality. A referral must be made to Children’s Services about the unborn child. If the woman is under 18 years then consideration will be given to whether she is a Child in Need. If she is less than 16 years then a criminal offence may have been committed and needs to be investigated. The reasons will not be known until there has been an assessment. If there is a denial of pregnancy then consideration must be given at the earliest opportunity to a referral for Mental Health Services. |
Education | |
| 1.7.11 | In many instances staff in educational settings may be the professionals who know a young person best. There are several signs to look out for that may give rise to suspicion of concealed pregnancy:
Staff working in educational settings should try to encourage the young person to discuss her situation as they would any other safeguarding concern. Every effort should be made by the professional suspecting a pregnancy to encourage the young person to obtain medical advice. However where they still face total denial or non-engagement further action should be taken. It may be appropriate to involve the assistance of the Safeguarding Lead or School’s Designated Safeguarding Lead in addressing these concerns. Consideration must be given to the balance of confidentiality and the potential concern for the unborn child and the mother’s health and well-being. Where there is a suspicion that a pregnancy is being concealed it is necessary to share this information with other agencies, irrespective of whether consent to disclose can be obtained. Education staff may often feel the matter can be resolved through discussion with the parent of the young person however this will need to be a matter of professional judgement (unless the young person has not given consent to tell the parents). It may be felt that the young person will not admit to her pregnancy because she has genuine fear about her parent’s reaction, or there may be other aspects about the home circumstances that give rise to concern. If this is the case a referral to Children’s Services must be made before disclosing the information about the pregnancy to her parents. If education staff do engage with parents they need to bear in mind the possibility of parent’s collusion with concealment. Whatever action is taken, the young person should be appropriately informed, unless there is a genuine concern that in so doing she may attempt to harm herself or the unborn baby. |
School Nursing | |
| 1.7.12 | The School Nurse may be well placed to identify and work with school age girls who may be pregnant by offering a confidential service. Boys as Father’s should also be considered. The School Nurse should liaise closely with the Teenage Pregnancy Midwives in order to support the young person having gained consent from the young person. If consent has not been obtained but there are still concerns for the young person/unborn child’s welfare, a referral to Children’s Services should be considered. |
Health | |
| 1.7.13 | If a health professional suspects or identifies a concealed or denied pregnancy a referral to Children’s Services must be made and all other health professionals that need to be involved in her care must also be informed. The health professionals whom may be involved include (list not exhaustive):
All health professionals should give consideration to the individual need of the young person to make or initiate a referral for a Mental Health Assessment at any stage of concern. Hospital Emergency Department staff or those in Radiology departments need to routinely ask women of child bearing age whether they might be pregnant. Health professionals who provide help and support to promote children’s or women’s health and development should be aware of the risk indicators and how to act on their concerns if they believe a young person may be concealing or denying a pregnancy. |
Midwives and Midwifery Services | |
| 1.7.14 | If an appointment for antenatal care has been made late (after 24 weeks) reasons for this must be explored. Midwives and Obstetricians should always consider whether there is a need for a referral to Mental Health Services. If a woman arrives at the hospital in labour or following an unassisted delivery, where a booking has not been made, then an urgent referral must be made to Children’s Services. The Emergency Duty team must be informed during the evening, on weekends or Public holidays. If the baby has been harmed in any way or there is a suspicion of harm, or the child is abandoned by the mother, the Police must be informed immediately and a referral made to Children’s Services. Midwives should ensure information regarding the concealed pregnancy is placed on the child’s, as well as the mother’s health records. Following an unassisted delivery or a concealed/denied pregnancy Midwives must be alert to the level of engagement shown by the mother, and her partner/extended family if observed, and of receptiveness to future contact with health professionals. In addition Midwives must be observant of the level of attachment behaviour demonstrated in the early postpartum period. In cases where there has been concealment and denial of pregnancy, especially where there has been unassisted delivery, consider a referral for a full Mental Health Assessment. In addition the baby should not be discharged until a multi-agency Strategy Meeting has been held and relevant assessments undertaken. A discharge summary from maternity services to primary care must report if a pregnancy was concealed or denied or booked late (beyond 24 weeks). |
GPs and Practice Employed Staff | |
| 1.7.15 | Women who are concealing are unlikely to present at GPs for pregnancy tests. However, they may present for another reason. As a matter of good practice, the possibility of pregnancy should be a prime consideration for GPs where nausea/vomiting is a key presenting symptom in a female patient who is of an age/development where sexual activity is possible. Appropriate examination and investigations should be performed. In some instances, women may be genuinely unaware they are pregnant, but in others, the woman may be determined to conceal the fact, and may be extremely reluctant to agree to a pregnancy test or examination. Where a GP has significant reason to believe a woman is pregnant, but further investigations are denied by the young person, action must be taken; where there are concerns about the potential welfare of the unborn child the GP should refer to Children’s Services. Given that a previous concealed pregnancy indicates increased risk of further concealment, where this has been the case it should be documented within the GP records. The GP may initiate a psychiatric assessment or be asked to make a referral by a colleague. |
Health Visitors/Family Nurses | |
| 1.7.16 | Health Visitors/Family Nurses in the course of their involvement with families will be aware of the circumstances of previous pregnancies and need to be alert to the possibility that a woman may be concealing a pregnancy. If the Health Visitor/Family Nurse believes the woman may be pregnant, they should encourage her to seek support. As an initial step it may be helpful to discuss the matter with the Named Nurse for Safeguarding Children, the GP and liaise with the Midwife to consider a way forward or a referral to Children’s Services made if there is total denial of the pregnancy.
|
Mental Health and Learning Disability Services | |
| 1.7.17 | Professionals working in mental health and learning disability may be more likely to be involved with a woman/young person who is concealing a pregnancy than other agencies. Mental illness, emotional problems, personality problems, a learning disability or substance misuse may all be contributory factors for concealment. If any professional working within these services identifies, or suspects a concealed pregnancy, they should seek to discuss this with the woman/young person, as appropriate, and contact their GP and/or Midwifery Services. |
Children's Services | |
| 1.7.18 | Where the expectant mother is under the age of 18 initial approaches should be made to discuss concerns regarding the potential concealed pregnancy and unborn child. Social Workers should take measured steps to ensure that the young person is not pregnant via appropriate medical examination or investigation, or to make realistic plans for the baby, including informing her parents. In all cases a multi-agency discussion should be held, involving all the relevant agencies, to assess the information and formulate a plan. A Pre-Birth Assessment will be undertaken. In the event that the young person refuses to engage in constructive discussion, and where parental involvement is considered appropriate to address risk, the parent/main carer should be informed and plans made wherever possible to ensure the unborn baby’s welfare. Potential risks to the unborn child or to the health of the young woman would outweigh the young person’s right to confidentiality, if there was significant evidence that she was pregnant. There may be significant reasons why a young woman may be concealing a pregnancy from her family and a Social Worker may need to consider speaking to her without her parent’s knowledge in the first instance. If the young woman refuses to engage in constructive discussion then the Social Worker will need to inform her parent/s or carers and continue to assess the situation with a focus on the needs /welfare of the unborn baby as well as those of the young woman, who should be considered a Child in Need. Where there are additional concerns (to the suspected concealed or denied pregnancy) such as a lack of engagement, possibility of sexual abuse, or substance misuse; a Section 47 Enquiry should be undertaken. An outcome of this may be to convene an Initial pre-birth Child Protection Conference. Where a woman under age 18 is suspected of being pregnant it must be recognised that she is also a Child in Need. If a young person has arrived at hospital either in labour (when a pregnancy has been concealed or denied) or following an unassisted birth an initial assessment must be started and a multi-agency Strategy Discussion held. In all cases the need to convene a Child Protection Conference must be considered. Any referral received by the Emergency Social Work Team in relation to a baby born following a concealed or denied pregnancy, or where a mother and baby have attended hospital following an unassisted delivery, then steps may need to be taken to prevent the baby being discharged from hospital until a multi-agency Strategy Discussion / Meeting has been held and a plan for discharge agreed. This would ordinarily be done by voluntary agreement with the woman, although clearly circumstances may arise when it may be appropriate to seek the assistance of the Police to prevent the baby from being removed from the hospital or an application made to seek an Emergency Protection Order. In undertaking an assessment the Social Worker will need to focus on the facts leading to the pregnancy, reasons why the pregnancy was concealed and gain some understanding of what outcome the mother intended for the child. These factors along with the other elements of the Assessment Framework will be key in determining risk. Accessing psychological services in concealment and denial of pregnancy may be appropriate and consideration should be given to referring a woman for psychological assessment. There could be a number of issues for the woman which would benefit from psychological intervention. A psychiatric assessment might be required in some circumstances, such as where it is thought she poses a risk to herself or others or in cases where a pregnancy is denied. The pathway for psychological or psychiatric assessment, either before or after pregnancy is the same. A referral should be made using the single point of entry to Mental Health Services and the referral letter copied to the young person’s GP. The referral should make clear any issues of concern for the young person’s mental health and issues of capacity. |
Police | |
| 1.7.19 | Thames Valley Police will be notified of any child protection concerns received by Children’s Services where concealment or denial of pregnancy is an issue. A Police representative will be invited to attend a multi-agency Strategy Meeting and consider the circumstances and to decide whether a joint Section 47 Enquiry should be carried out. Factors to consider will be the age of the person whom is suspected or known to be pregnant, and the circumstances in which she is living to consider whether she is a victim or potential victim of criminal offences. In all cases where a child has been harmed, been abandoned or died, Police and Social Care will work together to investigate the circumstances. Where it is suspected that neonaticide or infanticide has occurred then the Police will be the primary investigating agency. |
Referral where vulnerability is indicated
| 1.7.20 | If vulnerability is identified, early referral to appropriate support services will promote positive working relationships between both parents and key professionals. Early referrals can also help to ensure there is clarity around roles and responsibilities, and that appropriate early help and support is provided when considering the birth plan. Early assessment of need and the identification of appropriate support services is good practice and ensures that a planned and structured approach is taken and parents feel fully supported and are clear that if there are any concerns, what these are and how they will be addressed from the beginning of the process. At the beginning of any intervention it is important to identify whether the pregnant woman has any communication needs. At the earliest opportunity, access to translation or advocacy services should be considered. If at any stage it becomes known that a pregnancy is no longer viable this information needs to be sensitively communicated in a timely manner to all involved agencies and consideration given to referral for access to bereavement support for parents as appropriate. |
Early Help assessment and support
| 1.7.21 | Early intervention is essential in ensuring that unborn babies for whom risks or support needs are identified are given the best possible chances to reduce the need for statutory intervention. The outcome of this work will determine whether a referral to Children’s Services is necessary. Any intervention should be considered taking into account the thresholds laid down in Buckinghamshire’s Threshold document. The Continuum of Needs document will provide guidance on the types of family circumstances to be supported under Levels 1 – 4. If it has been identified that the parent/s may need additional support to meet the needs of their unborn child, this is the first stage in seeking to clearly identify these and the resources to address them. The Guidance in BSCP’s Early Help Strategy and the Referral Flowchart ‘What to do if you have a concern about a child in Buckinghamshire’ should be followed. If it is deemed appropriate through a multi-agency decision to manage the case via a ‘Family Plan’, a robust Early Help assessment should be completed by the lead professional identified and an early help plan developed. The development of an Early Help assessment and plan should follow the same principles of active multi-agency collaboration, planning and review as advocated in this procedure. Contributing professionals should be mindful that the Early Help plan may form the evidential basis for future intervention to safeguard the child either before or after birth. The early help planning and review process needs to be clear and robust. Given the relatively short timescale of the pregnancy, the decisions regarding the effectiveness and impact of an Early Help plan should be tightly managed. If it becomes evident that an Early Help plan is not having the desired impact because a parent is either not engaging with the plan, requires a more intensive plan, or steps need to be taken to safeguard the unborn child; a referral should be made to Children’s Services. If consent cannot be obtained for an early help assessment and plan, then a decision will need to be made as to the impact of not receiving services and whether this would escalate concerns to the threshold of risk of significant harm or whether there are enough strengths, support and monitoring in place to work at a universal level. |
Risk of significant harm
| 1.7.22 | Where there may be multiple vulnerabilities experienced by a family which could put the unborn baby, or the child once born, at risk of significant harm, a referral to Children’s Services should be made at the earliest opportunity in order to :-
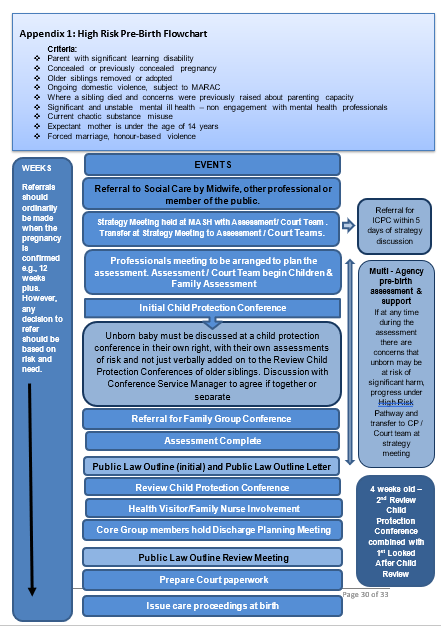
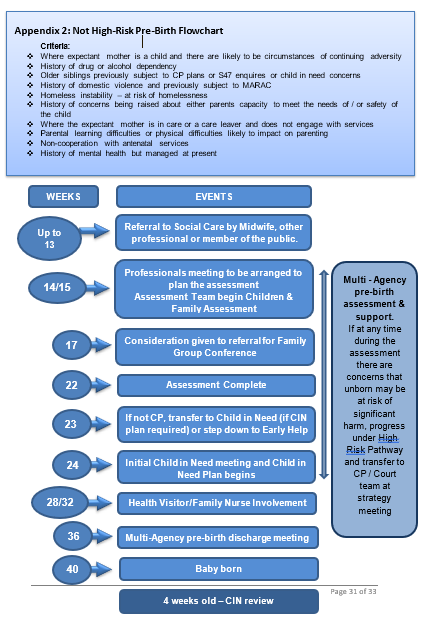
All referrals to Children’s Services should be made via the Multi-Agency Referral Form (MARF). Upon receipt of the referral, the Multi Agency Safeguarding Hub (MASH) will make a decision as to how to proceed and decide which service is appropriate to safeguard the unborn child. Decisions will be based on the presenting evidence and the threshold criteria. The referrer will receive feedback on what action is to be taken within one working day. If the parents are looked after children or care leavers and have had previous children removed from their care or the unborn has siblings currently subject to care proceedings or where the referral identifies significant risk of harm which might include: significant history of domestic abuse, parental mental health, significant drug use or homeless, the unborn child will be transferred to the Court Team for assessment. Allocation to the Court Team does not necessarily result in the Local Authority issuing care proceedings at birth. It reduces the changes of social worker and teams during the pregnancy stage and therefore the risk of drift and delay in care planning for the unborn. If the decision is taken that an assessment is required, the unborn child will follow one of two Pathways (see flowchart in Appendix 1 to this document). If the decision is taken that an assessment is required, the unborn child will follow one of two Pathways (see flowchart in Appendix 1 to this document).
If a Looked After Child becomes pregnant and a pre-birth assessment is required, the allocated social worker for that young person or health professional should make a referral to the MASH. Where one or both young persons are currently known to Children’s Services in their own right (i.e. subject to a Child in Need/Child Protection Plan, is a child looked after or a care leaver) then there will be a requirement of Children’s Services to assess the needs of the unborn baby and those of the pregnant young mother and putative father. The unborn baby be allocated their own Social worker and it will be an expectation that the that Social workers work closely together to share information about risks and support needs to ensure the safety of the unborn. Roles and responsibilities of each social worker (i.e. social worker for unborn and social worker for pregnant mother and putative parent/s) need to be agreed within the planning process, ensuring all partner agencies and professionals are aware of this so that there is clear communication. |
Family Group Conferences | |
| 1.7.23 | A Family Group Conference (FGC) should take place where there is a possibility that parents may require support in caring for the baby may not be able to care for baby. FGC is a forum to discuss the Local Authority’s worries and to enable the whole family network to consider how they can support the parent/s to be and the baby following birth within the family network. Holding a FGC will allow the family to engage in planning for the expected child and to identify what support is realistically available from the extended family or friends. Early identification of significant adults or family members who might be able to support or provide primary care is essential. They agree and develop a plan which will is owned by them. The family plan will address the future arrangements for the baby to ensure that they are adults who can safeguard and will be able to understand and the well being for the baby to remain within the family. their well-being is promoted. |
ReConnect - Oxford Health - (Improving relationships between parents and children) | |
| 1.7.24 | ReConnect is a service aimed at improving outcomes for the most vulnerable children under the age of two. This group will include children, as well as any unborn children, who are at high risk of developing a disorganised attachment through experiencing parenting breakdown, neglect and abuse, or parental mental health problems that impact on the child’s emotional needs. ReConnect aims at breaking the cycle of repeated abuse and neglect through offering intensive early intervention to high risk parents of all ages. ReConnect will work alongside multi-agency partners as part of the pre-birth assessment (as part of Child Protection plan or in Pre Proceedings) and provide early intervention that may improve the parenting capacity of mothers and improve the likelihood of them being able to parent their baby when born. In situations where a mother is unable to show sufficient improvement in her parenting and her baby is removed and permanently placed away from parents, ReConnect can continue with their work in the hope that improvements can be made in time for any future pregnancies. ReConnect will work with mothers with learning difficulties and will tailor their work to suit the mother’s level of understanding. |
Parents and child placements | |
| 1.7.25 | Consideration can be given to the suitability for a parent and child placement as soon as professionals become aware of the pregnancy. A parent and child placement is a fostering arrangement where a parent and their child are placed together in a fostering family. The placement is usually made following the birth of a baby with the aim of supporting the mother to develop the parenting skills needed to care for their baby and the ability to put the needs of their baby first. Placements are also offered to fathers and babies if the father is to be the main carer. The Fostering Service should be contacted for further consultation, when discussing suitability of a parent for a parent and child placement. In the event that there are suitable vacancies, a worker should be invited to the looked after child /permanency planning meetings to discuss plans for the child when born. Placements will be made voluntarily with the agreement of the parent(s), however most placements are made as a result of care proceedings and decisions made at court. The reasons when a parent and child placement may be considered suitable are when: There is a young parent or child in care indicating they may need support
Referrals to the Fostering Team for a parent and child placement can be made for cases that are currently open to Children’s Services for:
The Social Worker is aware of the requirements of parent and child placements, having attended the training and can provide the proactive support necessary in the early stages of the placement |
Midwifery and Children's Services Liaison meetings | |
| 1.7.26 | A High Risk pregnancy multi-agency meeting is held monthly, coordinated by a social worker from the court team. Professionals provide a short overview of their involvement with the family they wish to discuss, what their views are and what further information they require. This includes those where professionals are considering a social care referral, or have been referred to Children’s Service. The discussions enable an update to be shared amongst professionals on their assessments, planning and support being offered to parents. Unborn babies are discussed in detail after 24 weeks gestation (typically through Child in Need or Child Protection intervention) and a general overview discussion takes place on unborn babies after 13 weeks gestation. Complex assessments can be discussed in detail earlier than 24 weeks to ensure effective planning, these are reviewed by social care on an individual basis. These meetings also provide an opportunity to offer consultation on safeguarding issues including thresholds. Following these meetings, professionals are able to contact social care for any further discussions regarding any families. |
Where family plan to move or have moved at any point in the process | |
| 1.7.27 | Where there are significant concerns and the whereabouts of the mother are not known, the details must be passed to the Local Authority Child Protection Business Support Specialist team and the Designated Manager will ensure that other agencies and local authorities are informed in accordance with the procedures about a missing child, adult or family. Where there are significant concerns and the case is being transferred to another local authority, procedures across authorities must be followed. Transfer should not deter the originating authority from initiating or continuing Care Proceedings. In those circumstances, legal advice needs to be sought around jurisdiction issues and appropriate transfer points. |
Post Birth Planning
| 1.7.28 | Early planning is essential, particularly if there is a risk of baby being born pre-term. There should be a multi-agency meeting at 36 weeks which includes ward staff and any other professionals who may be relevant to the plan, immediately after birth. This meeting should ensure that there are plans that predict possible developments when the baby is born, including commencing Care Proceedings, seeking an Emergency Protection Order or Police Protection; in case parental agreement is withdrawn unexpectedly If abduction is a possibility the contingency planning for this would not be shared with the family. The Child Protection Plan/Discharge plan should always address the following issues:
Where vulnerability is identified late in the pregnancy it is essential that there is a clear plan regarding the birth of the baby. It is crucial that hospital discharge arrangements are clarified at the earliest opportunity. |
Related Policies, Procedures and Guidance
Useful References
Assessing Parents’ Capacity to Change: A Structured Approach. Frontline Briefing. Research in Practice/Dartington. 2013
Ages of concern: learning lessons from serious case reviews: A thematic report of Ofsted’s evaluation of serious case reviews from 1 April 2007 to 31st March 2011. Ofsted:
Brown L, Moore S and Turney D (2012) Analysis and Critical
Thinking in Assessment: Revised (2014) by Brown. L and Turney, D. Dartington: Research in Practice.
Children’s Needs – Parenting Capacity. Child Abuse: Parental mental illness, learning disability, substance misuse and domestic violence. 2nd Edition, London, The Stationery Office. (2011)
Domestic Violence and Pregnancy. www.refuge.org.uk
Fowler, J (2003) A Practitioner’s Tool for Child Protection and the Assessment of Parents. Jessica Kingsley Publishers: London.
Hart, Di (2000), Assessment Before Birth’ in Howarth, Jan (Ed) (2010) ‘The Child’s World Second Edition: The Comprehensive Guide to Assessing Children In Need’, Jessica Kingsley Publishers, London, (Chapter 14);
Huth-Bocks (2004). The impact of domestic violence on mothers’ prenatal representations of their infants, Infant Mental Health Journal, Michigan USA
Hart, Di (2001) and (2010), Assessment Prior to Birth’ in Howarth, Jan (Ed) (2010) ‘The Child’s World: Second Edition: The Comprehensive Guide to Assessing Children In Need’, Jessica Kingsley Publishers, London, (Chapter 14)
Hidden Harm – Responding to the needs of children of problem drug users. 2003
Information Sharing: Advice for practitioners providing safeguarding service to children, young people, parent and carers. DfE 2015.
Munro E (2011) The Munro Review of Child Protection: Final report. A child-centred system. London: Department for
Education.
NICE: Pregnancy and complex social factors – a model for service provision for pregnant women with complex social factors (2010) NICE guidelines CG110.
Population Matters: Teenage Pregnancy in England and Wales. May 2016
Reder, P. and Duncan, S. (1999) Lost innocents: a follow-up study of fatal child abuse, London: Routledge.
Rayna,G. Dawe, S and Cuthbert, C. (2011) All babies count: Spotlight on drugs and alcohol. NSPCC
Shemming, D, Rayns, G, Rickman, C and Mountain, G. (2016). Attachment: Understanding and supporting parent/carer bonding before birth and in infancy. Research in Practice.
Safeguarding Children and Young People from Sexual Exploitation: Supplementary guidance to Working Together to Safeguard Children
Turney, D. Analysis in Critical thinking in Assessment: A literature review. Dartington. RiP 2014
Wallbridge, S. Guide to pre-birth assessments. CC Inform. March 2012 (Reviewed March 2016).
Working Together to Safeguard Children: A guide to inter-agency working to safeguard and promote the welfare of children, March 2015.
Engaging men in the life of their families- a practice agenda can be found in A Framework for conducting Pre-Birth assessments: Martin C Calder: 2008. This document also includes over 20 other references for practice guidance and research papers, so provides excellent source material in this area of work.
Appendix
| 1.7.29 |
|
| 1.7.30 |
|
| 1.7.31 |
|